A twenty-one-year-oldgirl came with progressive diminution of vision. Initially, -2 diopters spherical lenses were prescribed. Anewpair of glasses were prescribed to her at every visit to optometrist due to a rapid progression of the myopia, which reached the value of -6 D when she was seven years old.
Figure 1: Image showing subluxated lens in the left eye
On Ophthalmological examination, best corrected vision was finger counting one meter in right eye and 6/18 in left eye with -6D spherical lenses i.e. high myopia was documented. The keratometry value of the right eye was 41.00 D and for the left eye it was 41.25 D. Axial lengthwas 25mm in both the eyes. On anterior segment examination, there was supero-nasal subluxationof the clear lens (Figure 1). The fundus was normal in both the eyes. We also notedtall stature, thinness (Size =1.40 m, weight = 25 kg for a Body Mass), arachnodactyly, a longer upper limb (Figure 2 and 3). Further history from parents revealed exceptional flexibility of the joints of this girl, as well as its large size compared to other children of the same age in the family. There was no history of similar complaints in any of the family member.
Figure 2: image showing Arachnodactyly
Patient was referred to physician examination for any systemic manifestations.
The systemic examination was normal. Diagnosis of marfan syndrome was made on the basis of these features.
Vitrectomy with lensectomy and scleral fixated intraocular lens was carried out on the right side. The post-operative period was uneventful. After six months, patient presented with diminution of vision in the right eye which was sudden in onset and was painless. On examination, best corrected vision was hand movement close to face. Anterior segment was normal. On fundus examination, Rhegmatogenous retinal detachment was documented in the right eye and surgerywas done. Patient had raised intraocular pressure after surgery andwas started on antiglaucoma medications (Figure 4). At present, patient does not perceive light in the right eye and the best corrected vision was 6/36 in the left eye. Most recent cardiovascular evaluation was normal.
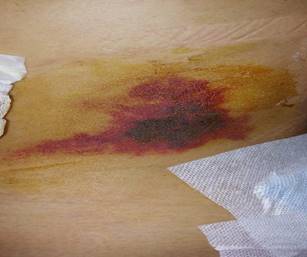
Figure 3: Dysmorphic facial features
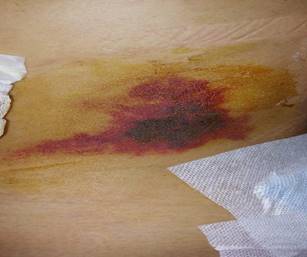
Figure 4: Right eye